|
Asthma Is a Serious Lung Disease
What Causes Asthma?
Your Asthma Can Be Controlled With Proper Care
How To Take Care of Your Asthma
How To Work With Your Doctor
Is Your Ashma Under Control?
Taking the Right Medicines at the Right Times
Asthma Medicines: Brand and Generic Names
How to Use Your Metered-Dose Inhaler the Right Way
Asthma Action Plan -
Printable form
How to Use Your Peak Flow Meter
How to Control Things That Make Your Asthma Worse
For More Information
If you have asthma, you are not alone. More than 14 million people in the United
States have this lung disease. Of these, almost 5 million are children. Asthma
is a problem among all races. But the asthma death rate and hospitalization rate
for blacks are three times the rate of whites. Proper asthma care could prevent
these problems for all.
 This website can help you learn how to control
your asthma or help a friend or family member with asthma. Asthma This website can help you learn how to control
your asthma or help a friend or family member with asthma. Asthma
Asthma Is a Serious Lung Disease
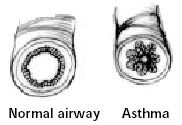
Asthma makes the sides of the airways in your lungs inflamed or swollen all the
time. See the drawing below. Your airways react to things like smoke, dust,
pollen, or other things. Your airways narrow or become smaller and you get
common symptoms like those listed in the box. Asthma that is not well controlled
can cause many problems. People miss work or school, go to the hospital, or even
die because of their asthma. But you do not have to put up with the problems
asthma can cause.
What Causes Asthma?
The cause of asthma is still unknown. From studying asthma patients, researchers
have concluded that the following factors can lead to asthma:
Genetic Factors: Asthma has the tendency to run in families. It
has not yet been determined what genetic factors actually play a part in
determining if a person will be diagnosed with asthma. Individuals who have
allergies are more likely to have asthma as well.
Air Quality: General environmental factors such as house dust
mites in bedding, carpet ad furnishings, exposure to tobacco smoke during
pregnancy or as a small child, and children who are exposed to animals, pollens,
molds and dust are more likely to have asthma. The occupational environment also
has a large influence on our likelihood of having asthma. Pollens, molds, dust,
gases and chemicals can cause our airways to become weak. The following are some
examples of hazardous occupations likely to cause asthma: manufacturing,
woodworking, farming and working with chemicals.
Dietary Changes: An increase in processed food, increase in
salt intake, decrease in antioxidant intake and the lack of fresh oily fish may
all increase the chances of cause asthma.
Lack of exercise: In the 21st century there has been an
increase in the amount of television that is watched and a decrease in the
amount of physical activity. This decrease in physical activity can cause a
decrease in the strength of the airway passage causing the airway muscles to
abnormally contract when irritated by environmental changes.
<<Back to Top>>
Your Asthma Can Be Controlled With Proper Care
With your doctor’s help, you can control your asthma and become free of symptoms
most of the time. But your asthma does NOT go away when your symptoms go away.
You need to keep taking care of your asthma.
Your asthma cannot be cured—having asthma is a part of your life. So you need to
make taking care of your asthma a part of your life. This is true even if your
asthma is mild.
<<Back to Top>>
How To Take Care of Your Asthma
- Work with your doctor and see him or her at least every 6 months.
See: “How To Work With Your Doctor”
- Take your asthma medicines exactly as your doctor tells you.
See: “Taking the Right Medicines at the Right Times”
“How To Use Your Metered-Dose Inhaler the Right Way”
“Asthma Action Plan”
- Watch for signs that your asthma is getting worse and act quickly.
See: “Asthma Action Plan”
(The action plan gives you some signs that your asthma is getting worse and says
when to take medicines.)
“How To Use Your Peak Flow Meter”
- Stay away from or control things that make your asthma worse.
See: “How To Control Things That Make Your Asthma Worse”
How To Work With Your Doctor
- Agree on clear treatment goals with your doctor. Your goal is to be able to say
“no” to all the questions in the box on section titled, “Is Your Asthma Under Control?”
- Agree on what things you need to do. Then do them.
- Ask questions until you feel you know what your doctor wants you to do, when
you should do it, and why. Tell your doctor if you think you will have trouble
doing what is asked. You can work together to find a treatment plan that is
right for you.
- Write down the things you are supposed to do before you leave the doctor’s
office, or soon after.
- Put up reminders to yourself to take your medicine on time. Put these notes in
places where you will see them.
- See your doctor at least every 6 months to check your asthma and review your
treatment. Call for an appointment if you need one.
Prepare a day or two before each doctor’s visit:
- Answer the questions in “Is Your Asthma Under Control?”.
Talk to your doctor about your answers. Also, talk about any changes in your
home or work that may have made your asthma worse.
- Write down questions and concerns to discuss with your doctor. Include ALL of
your concerns, even those you think are not a big deal.
- Bring your medicines and written action plan to each visit. If you use a peak
flow meter, bring it to each visit.
“The doctor would ask me at each visit how little Jimmy’s asthma was. I
always forgot to mention some symptoms or other problems. Now it’s different.
Before we visit the doctor, I write down when Jimmy had symptoms in the past 2
weeks. I also write down all the questions I have. Now when I leave the doctor’s
office, I feel happy that I got all my issues addressed.”
- Deborah, mother of a child with asthma
Is Your Ashma Under Control?
Answer these questions by checking "yes" or "no." Do this just before each
doctor's visit.
In the past 2 weeks
|
|
1. Have you coughed, wheezed, felt short of breath, or had chest tightness:
|
|
- During the day?
|
______ Yes
|
______ No
|
|
- At night, causing you to wake up?
|
______ Yes
|
______ No
|
|
- During or soon after exercise?
|
______ Yes
|
______ No
|
|
2. Have you needed more "quick-relief" medicine than usual?
|
______ Yes
|
______ No
|
|
3. Has your asthma kept you from doing anything you wanted to do? |
______ Yes
|
______ No
|
|
If yes, what was it?
|
|
|
|
____________________________________________________________ |
|
____________________________________________________________ |
|
4. Have you asthma medicines caused you any problems, like shakiness, sore
throat, or upset stomach?
|
______ Yes
|
______ No
|
|
In the past few months:
|
|
|
|
5. Have you missed school or work because of you asthma? |
______ Yes
|
______ No
|
|
6. Have you gone to the emergency room or hospital because of your asthma? |
______ Yes
|
______ No
|
|
|
What Your Answers mean
|
|
|
- All "no" asnwers? - Your asthma is under control.
- One or more "yes" answers? - Something needs to be done. Read
the guide on how to get your asthma under control and talk to your doctor.
|
|
|
Taking the Right Medicines at the Right
Times
There are two main kinds of medicines for asthma:
(1) those that help with the long-term control of asthma and
(2) those that give short-term quick relief from asthma symptoms.
See the list of brand and generic names for asthma
medicines.
Long-Term-Control Medicines Are Taken Every Day To Control Asthma
Long-term-control medicines will prevent symptoms and control asthma. But it
often takes a few weeks before you feel the full effects of this medicine.
Ask your doctor about taking daily long-term-control medicine if you:
- Have asthma symptoms three or more times a week, or
- Have asthma symptoms at night three or more times a month.
If you need a long-term-control medicine, you will need to keep taking your
medicine each day, even when you feel well. This is the only way you can keep
your asthma under control. Make taking your long-termcontrol medicine a part of
your daily routine—just like eating, sleeping, and brushing your teeth.
The Long-Term-Control Medicines
The most effective long-term-control medicines are those that reduce swelling in
your airways (inflammation). These medicines include inhaled steroids, cromolyn,
and nedocromil.
- Inhaled steroids and steroid tablets or liquids are the strongest
long-term-control medicines. The steroids used for asthma are NOT the same as
the unsafe steroids some athletes take to build muscles.
- Inhaled steroids are used to prevent symptoms and control mild, moderate, and
severe asthma. Inhaled steroids are safe when taken at recommended doses. This
is because the medicine goes right to your lungs where you need it. This reduces
the amount of medicine you need and the chance of any side effects.
- Steroid tablets or liquids are used safely for short times to quickly bring
asthma under control. They are also used longer term to control the most severe
asthma.
- Cromolyn and nedocromil are often the choice of medicine for children with mild
asthma.
- Inhaled long-acting beta2- agonists are used to help control moderate-to-severe
asthma and to prevent nighttime symptoms. Long-acting beta2-agonists do not
reduce inflammation. Therefore, patients taking this medicine also need to take
inhaled steroids. Inhaled longacting beta2-agonists should not be used for quick
relief of asthma attacks.
- Sustained-release theophylline or sustained-release beta2- agonist tablets can
help prevent nighttime symptoms. These medicines are used with inhaled steroids,
nedocromil, or cromolyn. Theophylline is sometimes used by itself to treat mild
asthma. The dose for theophylline must be checked over time to prevent side
effects.
- Zileuton and zafirlukast are a more recent type of long-termcontrol medicine.
Studies so far show that it is used mainly for mild asthma in patients 12 years
of age and older.
Quick-Relief Medicines Are Taken Only When Needed
Inhaled quick-relief medicine quickly relaxes and opens your airways and
relieves asthma symptoms. But it only helps for about 4 hours. Quick-relief
medicine cannot keep symptoms from coming back—only long-termcontrol medicines
can do that.
Take quick-relief medicine when you first begin to feel symptoms— like coughing,
wheezing, chest tightness, or shortness of breath. Your doctor may tell you to
use a peak flow meter to help you know when to take your inhaled quickrelief
medicines. Do not delay taking your quickrelief medicine when you have symptoms.
This can keep you from having a really bad asthma attack. Tell your doctor if
you notice you are using more of this medicine than usual. This is often a sign
that your long-term-control medicine needs to be changed or increased.
Make an Action Plan With Your Doctor
Ask your doctor to help you fill out the “Asthma Action Plan”. Be sure you know when to take your
medicine and what to do when your asthma gets worse.
“I always thought if you had asthma you should expect to have asthma
symptoms. My new doctor disagreed. She told me to take an “inhaled steroid”
every day for my asthma. Well, I did not feel anything at first. But after about
3 weeks, my symptoms came less often. Now, after a few months on this medicine,
I can see my doctor was right. Asthma can really be controlled.”
Glen, a long-time asthma patient
|
Asthma Medicines: Brand and Generic
Names, 1997*
|
|
Asthma Long-Term Control Medications
|
|
Generic Name
|
Brand Name
|
|
|
Steroids: Inhaled |
|
|
belomethasone |
Beclovent®
Vanceril®, Vanceril®—Double |
|
Strength |
|
|
budesonide |
Pulmicort Turbuhalor® |
|
flunisolide |
AeroBid®, AeroBid-M® |
|
fluticasone |
Flovent® |
|
triamcinolone |
Azmacort® |
|
|
Cromolyn and Nedocromil: Inhaled |
|
cromolyn sodium |
Intal® |
|
nedocromil sodium |
Tilade® |
|
|
Leukotriene Modifiers: Tablets |
|
zafirlukast |
Accolate® |
|
zileuton |
Zyflo® |
|
|
Long-Acting Beta2-Agonists |
|
salmeterol (inhaled)
|
Serevent® |
|
albuterol |
Volmax® |
|
(extended release tablets) |
Proventil Repetabs ® |
|
|
Theophylline: Tablets or liquid |
|
|
Aerolate® III
Aerolate® JR
Aerolate® SR
Choledyl® SA
Elixophyllin®
Quibron®-T
Quibron®-T/SR
Slo-bid®
Slo-Phyllin®
Theo-24®
Theochron®
Theo-Dur®
Theolair®
Theolair®-SR
T-Phyl®
Uni-Dur®
Uniphyl® |
|
|
Asthma Quick-Relief Medications |
|
Generic Name
|
Brand Name
|
|
|
Short-Acting Beta2-Agonists: Inhaled |
|
albuterol |
Airet®
Proventil®
Proventil HFA®
Ventolin®
Ventolin® Rotacaps |
|
bitolterol |
Tornalate® |
|
pirbuterol |
Maxair® |
|
terbutaline |
Brethaire®
Brethine® (tablet only)
Bricanyl® (tablet only) |
|
|
Anticholinergics: Inhaled |
|
ipratropium bromide |
Atrovent® |
|
|
Steroids: Tablets or liquids |
|
methylprednisolone |
Medrol® |
|
prednisone |
Prednisone
Deltasone®
Orasone®
Liquid Pred®
Prednisone Intensol® |
|
prednisolone |
Prelone®
Pediapred® |
|
|
|
|
* This glossary is a complete list of brand names associated with the
appropriate generic names of asthma medications, as listed in the United States
Pharmacopeial Convention, Inc., Approved Drug Products and Legal Requirements,
Volume III, 17th edition, 1997, and the USP DI Drug Information for Health Care
Professionals, Volume I, 17th edition, 1997. This list does not constitute an
endorsement of these products by the National Heart, Lung, and Blood Institute. |
|
|
How to Use Your Metered-Dose Inhaler the Right
Way
|
Using an inhaler seems simple, but most patients do not use it the right
way. When you use your inhaler the wrong way, less medicine gets to your lungs.
(Your doctor may give you other types of inhalers.)
For the next 2 weeks, read these steps aloud as you do them or ask someone
to read them to you. Ask your doctor or nurse to check how well you are using
your inhaler.
Use your inhaler in one of the three ways pictured below (A or B are best,
but C can be used if you have trouble with A and B). |
|
Steps for Using Your Inhaler
|
|
|
Getting Ready
|
1. Take off the cap and shake the inhaler.
2. Breathe out all the way.
3. Hold your inhaler the way your doctor said (A, B, or C below). |
|
Breathe in slowly
|
4. As you start breathing in slowly through your mouth, press down on the
inhaler one time. (If you use a holding chamber, first press down on the
inhaler. Within 5 seconds, begin to breathe in slowly.)
5. Keep breathing in slowly, as deeply as you can. |
|
Hold your breath |
6. Hold your breath as you count to 10 slowly, if you can.
7. For inhaled quick-relief medicine (beta2-agonists), wait about 1 minute
between puffs. There is no need to wait between puffs for other medicines. |
|
A. Hold inhaler 1 to 2 inches in front of your mouth (about the width of two
fingers). |
B. Use a spacer/holding chamber. These come in
many shapes and can be useful to any patient. |
C. Put the inhaler in your mouth. Do not use for steroids.
|
|
|
|
|
Clean Your Inhaler as Needed
Look at the hole where the medicine sprays out from your inhaler. If you see
“powder” in or around the hole, clean the inhaler. Remove the metal canister
from the L-shaped plastic mouthpiece. Rinse only the mouthpiece and cap in warm
water. Let them dry overnight. In the morning, put the canister back inside. Put
the cap on. |
Know When To Replace Your Inhaler
For medicines you take each day (an example): Say your new canister has 200
puffs (number of puffs is listed on canister) and you are told to take 8 puffs
per day.

So this canister will last 25 days. If you started using this inhaler on May 1,
replace it on or before May 25.
You can write the date on your canister. For quick-relief medicine take as
needed and count each puff.
Do not put your canister in water to see if it is empty. This does not work.
|
|
How to Use Your Peak Flow Meter
|
A peak flow meter helps you check how well your asthma is controlled. Peak flow
meters
are most helpful for people with moderate or severe asthma.
This guide will tell you (1) how to find your personal best peak flow number,
(2) how to use your personal best number to set your peak flow zones, (3) how to
take your peak flow, and (4) when to take your peak flow to check your asthma
each day. |
|
Starting Out: Find Your Personal Best Peak Flow Number |
|
To find your personal best peak flow number, take your peak flow each day for 2
to 3 weeks. Your asthma should be under good control during this time. Take your
peak flow as close to the times listed below as you can. These times for taking
your peak flow are only for finding your personal best peak flow.
- Between noon and 2:00 p.m. each day
- Each time you take your quickrelief medicine to relieve symptoms (measure your
peak flow after you take your medicine)
- Any other time your doctor suggests
Write down the number you get for each peak flow reading. The highest peak flow
number you had during the 2 to 3 weeks is your personal best.
Your personal best can change over time. Ask your doctor when to check for a new
personal best.
To check your asthma each day, you will take your peak flow in the morning. This
is discussed in the coming text.
|
|
Your Peak Flow Zones |
Your peak flow zones are based on your personal best peak flow number. The zones
will help you check your asthma and take the right actions to keep it
controlled. The colors used with each zone come from the traffic light. |
|
|
Green Zone (80 to 100 percent of your personal best) signals
good control. Take your usual daily long-term-control medicines, if you take
any. Keep taking these medicines even when you are in the yellow or red zones. |
|
|
Yellow Zone (50 to 79 percent of your personal best) signals
caution: your asthma is getting worse. Add quick-relief medicines. You might
need to increase other asthma medicines as directed by your doctor. |
|
|
Red Zone (below 50 percent of your personal best) signals
medical alert! Add or increase quick-relief medicines and call your doctor now. |
|
Ask your doctor to write an
action plan for you that tells you:
- The peak flow numbers for your green, yellow, and red zones. Mark the zones on
your peak flow meter with colored tape or a marker.
- The medicines you should take while in each peak flow zone.
How To Take Your Peak Flow
- Move the marker to the bottom of the numbered scale.
- Stand up or sit up straight.
- Take a deep breath. Fill your lungs all the way.
- Hold your breath while you place the mouthpiece in your mouth, between your
teeth. Close your lips around it. Do not put your tongue inside the hole.
- Blow out as hard and fast as you can. Your peak flow meter will measure how fast
you can blow out air.
- Write down the number you get. But if you cough or make a mistake, do not write
down the number. Do it over again.
- Repeat steps 1 through 6 two more times. Write down the highest of the three
numbers. This is your peak flow number.
- Check to see which peak flow zone your peak flow number is in. Do the
actions your doctor told you to do while in that zone.
Your doctor may ask you to write down your peak flow numbers each day. You can
do this on a calendar or other paper. This will help you and your doctor see how
your asthma is doing over time.
Checking Your Asthma: When To Use Your Peak Flow Meter
- Every morning when you wake up, before you take medicine. Make this part
of your daily routine.
- When you are having asthma symptoms or an attack. And after taking medicine for
the attack. This can tell you how bad your asthma attack is and whether your
medicine is working.
- Any other time your doctor suggests. If you use more than one peak flow meter
(such as at home and at school), be sure that both meters are the same brand.
Bring to Each of Your Doctor’s Visits:
- Your peak flow meter.
- Your peak flow numbers if you have written them down each day.
Also, ask your doctor or nurse to check how you use your peak flow meter—just to
be sure you are doing it right.
How to Control Things That Make Your Asthma
Worse
You can help prevent asthma attacks by staying away from things that make your
asthma worse. This guide suggests many ways to help you do this.
You need to find out what makes your asthma worse. Some things
that make asthma worse for some people are not a problem for others. You do not
need to do all of the things listed in this guide.
Look at the things listed in dark print below. Put a check next to the ones that
you know make your asthma worse. Ask your doctor to help you find out what else
makes your asthma worse. Then, decide with your doctor what steps you will take.
Start with the things in your bedroom that bother your asthma. Try
something simple first.
|
Tobacco Smoke
- If you smoke, ask your doctor for ways to help you quit. Ask family members to
quit smoking, too.
- Do not allow smoking in your home or around you.
- Be sure no one smokes at a child’s day care center.
Smoke, Strong Odors, and Sprays
- If possible, do not use a wood-burning stove, kerosene heater, or fireplace.
- Try to stay away from strong odors and sprays, such as perfume, talcum powder,
hair spray, and paints.
Indoor Mold
- Fix leaky faucets, pipes, or other sources of water.
- Clean moldy surfaces with a cleaner that has bleach in it.
|
Dust Mites
Many people with asthma are allergic to dust mites. Dust mites are like tiny
“bugs” you cannot see that live in cloth or carpet.
Things that will help the most:
- Encase your mattress in a special dust-proof cover.*
- Encase your pillow in a special dust-proof cover* or wash the pillow each week
in hot water. Water must be hotter than 1300F to kill the mites.
- Wash the sheets and blankets on your bed each week in hot water.
Other things that can help:
- Reduce indoor humidity to less than 50 percent. Dehumidifiers or central air
conditioners can do this.
- Try not to sleep or lie on cloth-covered cushions or furniture.
- Remove carpets from your bedroom and those laid on concrete, if you can.
- Keep stuffed toys out of the bed or wash the toys weekly in hot water.
|
|
Animal Dander
Some people are allergic to the flakes of skin or dried saliva from animals with
fur or feathers.
The best thing to do:
- Keep furred or feathered pets out of your home.
If you can’t keep the pet outdoors, then:
- Keep the pet out of your bedroom and keep the bedroom door closed.
- Cover the air vents in your bedroom with heavy material to filter the air.*
- Remove carpets and furniture covered with cloth from your home. If that is not
possible, keep the pet out of the rooms where these are.
|
Cockroach
Many people with asthma are allergic to the dried droppings and remains of
cockroaches.
- Keep all food out of your bedroom.
- Keep food and garbage in closed containers (never leave food out).
- Use poison baits, powders, gels, or paste (for example, boric acid). You can
also use traps.
- If a spray is used to kill roaches, stay out of the room until the odor goes
away.
Vacuum Cleaning
- Try to get someone else to vacuum for you once or twice a week, if you can. Stay
out of rooms while they are being vacuumed and for a short while afterward.
- If you vacuum, use a dust mask (from a hardware store), a double-layered or
microfilter vacuum cleaner bag,* or a vacuum cleaner with a HEPA filter.*
|
|
Pollen and Outdoor Mold
What to do during your allergy season (when pollen or mold spore counts are
high):
- Try to keep your windows closed.
- Stay indoors with windows closed during the midday and afternoon, if you can.
Pollen and some mold spore counts are highest at that time.
- Ask your doctor whether you need to take or increase anti-inflammatory medicine
before your allergy season starts.
|
Exercise, Sports, Work, or Play
- You should be able to be active without symptoms. See your doctor if you have
asthma symptoms when you are active—like when you exercise, do sports, play, or
work hard.
- Ask your doctor about taking medicine before you exercise to prevent symptoms.
- Warm up for about 6 to 10 minutes before you exercise.
- Try not to work or play hard outside when the air pollution or pollen levels (if
you are allergic to the pollen) are high.
|
|
Other Things That Can Make Asthma Worse
- Flu: Get a flu shot.
- Sulfites in foods: Do not drink beer or wine or eat shrimp, dried fruit, or
processed potatoes if they cause asthma symptoms.
- Cold air: Cover your nose and mouth with a scarf on cold or windy days.
- Other medicines: Tell your doctor about all the medicines you may take. Include
cold medicines, aspirin, and even eye drops.
|
Contact These Groups to Learn More About
Asthma:
<<Back to Top>>
|
|